Asthma in children under 6
11-minute read
Asthma can be life-threatening — if your child is finding it hard to breathe, take them to the nearest hospital emergency department or call triple zero (000) for an ambulance.
Key facts
- Asthma causes the small airways in your child’s lungs to narrow.
- Symptoms of asthma in young children include wheezing, difficulty breathing and cough.
- The most common trigger for asthma symptoms in young children is a viral infection, such as a cold.
- Allergies are also common in children with wheezing and asthma.
- It’s important that your child has a written asthma action plan to help manage their asthma.
What is asthma?
Asthma is a condition that causes wheezing and difficulty breathing. It can be mild or severe.
When you have asthma, the small airways in your lungs become narrowed from time to time. This is due to:
- the airways becoming swollen and inflamed
- the thin layer of muscle in your airways tightening
- the airways having mucus inside them
Wheezing is the most common symptom of asthma in children aged 5 years and under. Wheezing is a high-pitched sound coming from your child’s chest when they breathe in and out.
It’s important to know that not all pre-school aged children with wheezing will be diagnosed with asthma.
The information in this article focuses on asthma in children aged 0 to 5 years. For information on , visit healthdirect.
What are the symptoms of asthma in children?
Symptoms of asthma in children can include:
- episodes of wheezing
- — especially at night, in the early morning or when your child is active
- — this may be noticed when it limits your child’s activities
- chest tightness — this is when your child's breathing feels 'tight'
What causes asthma?
The exact cause of asthma is not known.
Asthma symptoms can be triggered by many things. The most common trigger is a viral infection, such as a .
Many children with asthma have:
- a of asthma or
- allergic conditions, such as or
Your child’s symptoms may be triggered by an allergy to:
- house
- (dead skin and fur), usually from pets
Other triggers for asthma include:
- exercise
- cold, dry air
- changes in the air environment (such as and smoke)
You can prevent asthma symptoms by helping your child avoid triggers when possible.
When should I see my doctor?
You should see your doctor if your child has wheezing or other symptoms of asthma.
When to seek urgent care
If your child is finding it hard to breathe, take them to the nearest hospital emergency department or call triple zero (000) for an ambulance.
Get urgent medical attention if your child has any of the following symptoms:
- difficulty breathing — you may see rapid breaths, inward movement of the chest wall when your child breaths in, and grunting while they breathe out
- unable to speak normally
- bluish lips — this is a sign that not enough oxygen is reaching their body
- tightness in their chest
- constant coughing or wheezing that does not get better with asthma medicines
Your child may appear distressed or tell you that they are having trouble breathing. A severe asthma attack is very upsetting because your child will feel that they are unable to get enough air.
How is asthma diagnosed?
Your doctor will ask about your child’s symptoms. It’s helpful if you can show the doctor a video of your child when they are wheezing.
Your doctor will want to know:
- what tends to bring on their wheezing
- whether your child has daytime or night-time symptoms
- how often your child has symptoms
- about your child’s general health, including any allergies
- whether you have pets
- whether anyone in your family has asthma or allergies
Your doctor will , including listening to their breathing with a stethoscope.
Your doctor may recommend tests, such as or a chest . They may also refer you to a (children’s doctor).
If your doctor thinks that your preschool-aged child may have asthma, they may start a treatment trial. This means that they will give your child asthma medicines to see if they help with their symptoms.
Spirometry can only be used to diagnose asthma in older children. Spirometry is a type of lung function test.
How is asthma treated?
The 2 main types of are known as 'relievers' and 'preventers'.
- Relievers help to ease the symptoms of asthma when they happen. The most commonly used reliever is (one brand is Ventolin, but there are others).
- Preventers help prevent episodes of asthma. Preventer medicines need to be taken every day, even when your child is feeling well. Some preventer medicines are taken as inhalers (breathed in through the lungs), while others are taken as a tablet.
Asthma medicines are often taken using an inhaler and a device called a spacer. It’s important to learn properly.
Your child will need regular follow-up visits with your doctor. This is to check on their symptoms and work out if treatment is still needed.
It can help to keep a diary to record symptoms and when asthma medicines are given. This can help your doctor know if changes to medicines are needed.
Many preschool children with wheezing do not have asthma by primary school age.
Asthma action plan
Ask your doctor to create a written asthma action plan for your child. The plan helps you manage your child’s asthma. It tells you:
- how to look after your child's asthma each day
- when and how they should take their medicine
- what to do if their symptoms get worse
Share your child’s asthma action plan with everyone who cares for your child. This includes childcare, friends and family members.
Managing an acute asthma attack
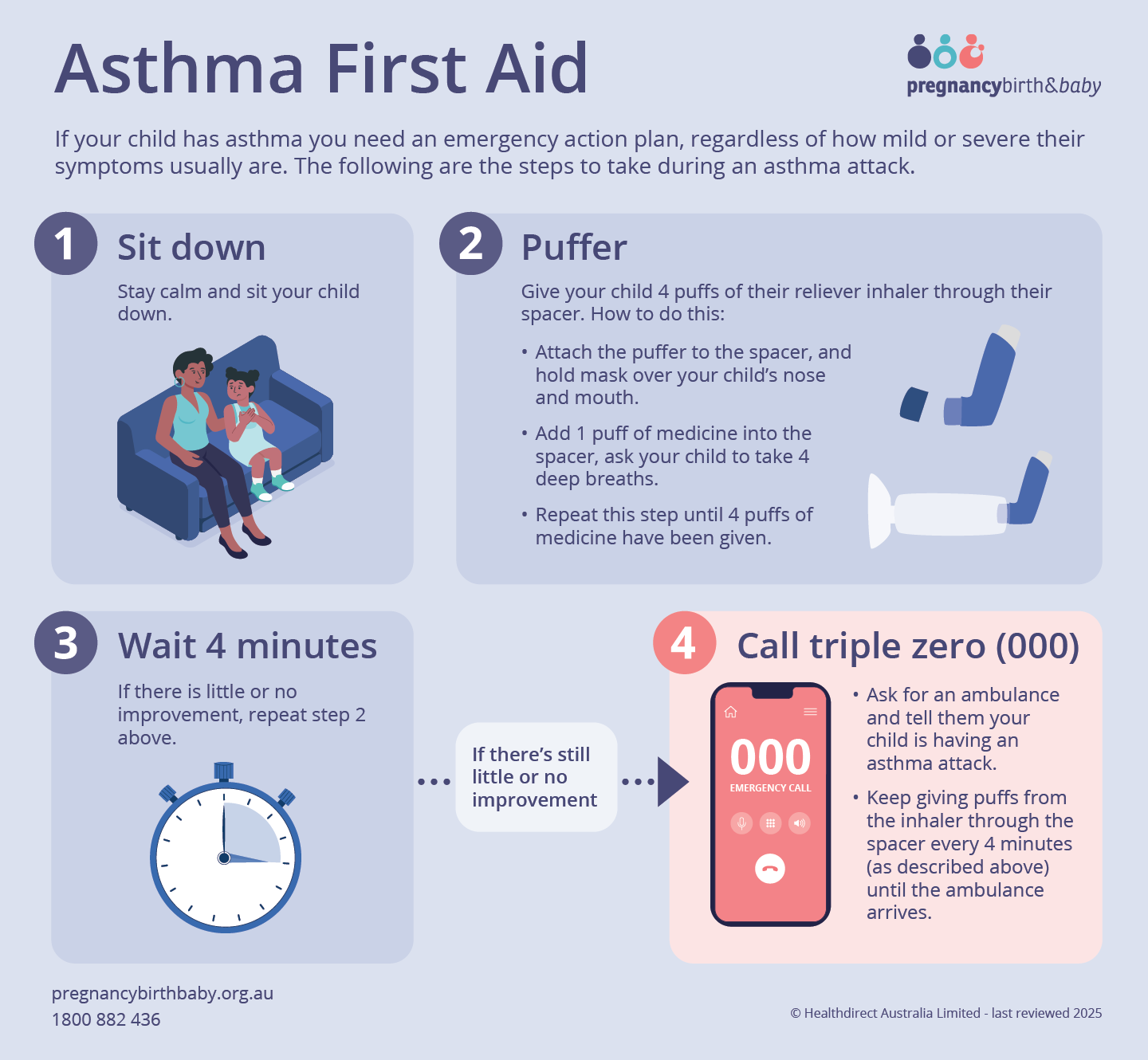
If your child has asthma, you need an emergency action plan, even if their symptoms are usually mild.
If your child has a severe asthma attack:
- Stay calm and sit your child down.
- Give your child 4 puffs of their reliever inhaler through their spacer. For each puff of medicine, your child should take 4 deep breaths before you give the next puff.
- Wait 4 minutes. If there is little or no improvement, repeat step 2 above.
- If there is still little or no improvement after 4 minutes, call triple zero (000) and ask for an ambulance. State that your child is having an asthma attack.
While waiting for the ambulance to arrive, give your child puffs from the inhaler through the spacer as described above. Wait 4 minutes and do it again. Repeat this until the ambulance arrives.
Can asthma be prevented?
It’s recommended that you avoid smoking while pregnant and make sure your baby is not exposed to cigarette smoke. This may help prevent asthma.
Asthma symptoms and asthma attacks can sometimes be prevented by avoiding triggers. For example, if you know that animal dander (dead skin and fur) triggers your child's asthma, removing or reducing animal hair in your home can help.
It’s also recommended that your child has a yearly flu vaccination.
What are the complications of asthma?
Children with asthma can have severe asthma attacks. Sometimes children with severe asthma symptoms need to go to the emergency department and stay in hospital for treatment.
It’s important to manage your child’s asthma well. This can help prevent frequent and severe symptoms and attacks.
Should my child with asthma be active?
It’s important that children with asthma are to help them stay .
Talk with your doctor about preventing and managing symptoms when your child is active. Your child's asthma management plan will help with this.
Resources and support
has:
- information on asthma and
- asthma
- videos on
- a fact sheet on
Call the on 1800 278 462 to talk to an Asthma Educator.
The Royal Children's Hospital Melbourne has a , available in different languages.
Log on to the to help keep track of your child's symptoms.
The National Asthma Council's ‘’ has practical strategies to help you understand and manage your child's asthma.

Speak to a maternal child health nurse
Call ºÚÁϳԹÏ, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2025


