Umbilical cord prolapse
10-minute read
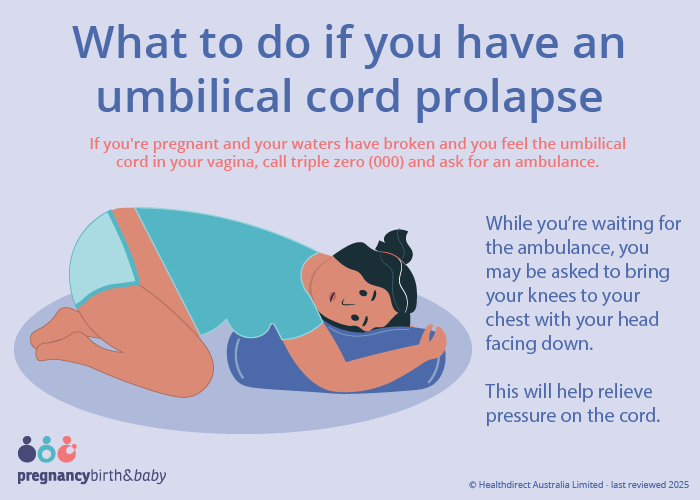
If you're pregnant and your waters have broken and you feel the umbilical cord in your vagina, call triple zero (000) and ask for an ambulance.
Key facts
- An umbilical cord prolapse is an emergency because it can reduce the flow of oxygen to your baby.
- It happens when the umbilical cord moves in front of your baby.
- You may feel or see the umbilical cord coming out of your vagina.
- You need to birth your baby safely and quickly — this is usually by an emergency caesarean section.
- Having an umbilical cord prolapse can be frightening — talk with your midwife or doctor about what happened.
What is an umbilical cord?
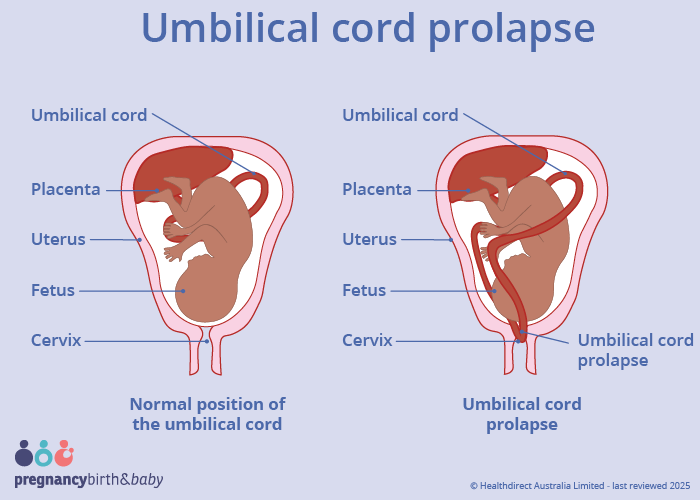
The umbilical cord connects your baby to the placenta in your uterus. The cord gives your baby nutrients and oxygen. It also takes waste products away.
What is an umbilical cord prolapse?
An umbilical cord prolapse (also known as 'cord prolapse') is when the umbilical cord moves in front of your baby. This means that the cord may pass through your cervix before your baby does, or together with your baby.
Cord prolapse usually happens during labour but, it can only happen once your waters have broken.
Cord prolapse is rare, happening in about 1 in 600 births.
What are the symptoms of an umbilical cord prolapse?
The symptoms of an umbilical cord prolapse are:
- feeling the cord in your vagina
- seeing the cord coming out of your vagina
- your midwife or doctor seeing the cord in your vagina
- a change in your baby's movements
- your baby's heart rate slowing
- meconium (your baby's poo) in your amniotic fluid
The umbilical cord is a shiny, blueish white colour.
Sometimes there are no signs of a cord prolapse.
If your baby is not positioned head down, you should go to hospital urgently if your waters break or you think you may be going into labour.
When should I call an ambulance or go to the emergency department is cord?
If you're pregnant and your waters have broken and you feel the umbilical cord in your vagina, call triple zero (000) and ask for an ambulance.
An umbilical cord prolapse is an emergency because it can reduce the flow of oxygen to your baby.
The umbilical cord may become compressed (squashed) between your baby and the birth canal. This reduces or stops the flow of blood in the cord.
While you're waiting for the ambulance, you may be asked to bring your knees to your chest with your head facing down. This will help relieve pressure on the cord.
What causes an umbilical cord to prolapse?
You're more likely to have an umbilical cord prolapse if:
- you've had one or more babies before
- you've had a baby that weighs less than 2.5kg at birth
- having too much amniotic fluid
- you have a different pelvic structure
The chance of umbilical cord prolapse increases if your baby:
- is not head down in the birth canal
- has birth differences (congenital anomalies)
- has a very long umbilical cord
- is the second twin in a twin pregnancy
- is premature
If you have any of these risk factors, your health team will check for cord prolapse every time you have a vaginal examination.
How is an umbilical cord prolapse diagnosed?
Your midwife or doctor will check for cord prolapse when they do a vaginal examination. This is done once your waters break or when you're in labour. If you are not yet in labour, they may use a speculum for this.
A change in your baby's heart rate may prompt your care provider to check for cord prolapse.
How is an umbilical cord prolapse treated?
Cord prolapse is a medical emergency.
An emergency caesarean section is usually recommended. Your midwife or doctor will explain the situation to you. They should ask for you to provide consent.
You may need a so your baby can be born more quickly.
Your midwife or doctor will gently lift your baby's head off the cord. This reduces the pressure on the cord.
They may also put a catheter into your bladder and fill it with water. This also helps to lift your baby's head off the cord.
In some situations, a vaginal or assisted birth may be possible if you're close to giving birth.
If you are in labour, you might be given medicines to stop your contractions.
You can read more about shared decision making.
What are the complications of an umbilical cord prolapse?
Having an umbilical cord prolapse can be frightening. Talk with your midwife or doctor about what happened. They can help answer your questions.
You may find it helpful to talk to a or counsellor. It's important to get support if you need it.
Your partner and family may also find it helpful to talk about what happened.
Find out more about traumatic birth experiences.
Is this likely to happen in future pregnancies?
You are unlikely to have a cord prolapse in future pregnancies.
Ask your doctor or midwife what they recommend for your next pregnancy.
Complications for my baby
Most babies will have no complications from an umbilical cord prolapse.
However, there's a chance that your baby may not have received enough oxygen. This can cause brain damage. It's very rare that a baby dies from cord prolapse.
Can an umbilical cord prolapse be prevented?
Umbilical cord prolapse can't be prevented.
If you have a higher chance of having a cord prolapse, you may be looked after in hospital.
Your midwife or doctor may recommend staying in hospital from 37 weeks of pregnancy, if:
- your baby is lying on its side (known as transverse or oblique presentation)
- your baby's position changes (known as mobile presentation)
That way help is at hand when your waters break or you go into labour.
Sometimes the cord is felt during a vaginal examination before your waters have broken. In such cases your doctor will not break your waters if possible.
Resources and support
For more information on umbilical cord prolapse read the .
Visit for information and support, including peer-to-peer support.
Australia offers both online and phone support for new parents. You can call them on 1300 851 758
offers mental health support and counselling — call 1300 22 4636 or chat to a counsellor online.

Speak to a maternal child health nurse
Call ºÚÁϳԹÏ, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2025


